INTRODUCTION
A developing economy needs high-level technical manpower as urgently as it needs capital. A crucial factor in improving the coverage and quality of health services is the availability of adequate number of health personnel with task-oriented training.
According to Dev Ray, “A health manpower plan is meant to ensure that the right number and quality of manpower are available to staff the health facilities as the needs expand, so as to keep up with current and future demands of services from the people.”1
HEALTH MANPOWER PLANNING
Manpower is the most crucial resource toward delivery of health planning. Manpower planning is a technique of correcting imbalances between manpower demand and manpower supply in the economy. Manpower planning is concerned not only with balancing of demand and supply of different categories of manpower, but also with the overall development and utilization of manpower resources in the country. The utilization of manpower is the process of matching men and work in accordance with their level of development. So it is an integrated approach that should not be considered isolated.
Health Manpower
Health manpower refers to people who are trained to promote health, to prevent and to cure disease, and to rehabilitate the sick.
The aim of manpower planning is to make available the right kind of personnel in the right number with appropriate skills at the right place at the right time doing the right job.
HUMAN RESOURCES FOR HEALTH
Trained and competent human resource is the foundation of an effective health system. Various types of health resources are doctors [allopathic and Ayurveda, Yoga and naturopathy, Unani, Siddha, and Homeopathy (AYUSH)], nurses, pharmacists, lab technicians, radiographer health assistants (male and female), health workers (male), auxiliary nurse midwife (ANM), accredited social health activists (ASHAs), anganwadi workers, trained dais, and others (health inspectors, health educators, occupational therapy assistant, dieticians, etc.).
Table 1: Suggested norms for health manpower
Source: Govt. of India (2008), Annual report 2007–2008, Ministry of Health and Family Welfare, New Delhi2
While Table 1 shows the suggested norms of health manpower required for provision of adequate health facilities, currently, various developing countries lag behind these suggested norms, including India. The current status of health manpower in various countries is shown in Table 2.
Presently, India produces 30,000 doctors, 18,000 specialists, 30,000 AYUSH graduates, 54,000 nurses, 15,000 ANMs, and 36,000 pharmacists annually. There has been a steady rise of allopathic doctors since 2008 (Graph 1).
Along with doctors, presently, admission capacity for nursing staff and pharmacists is also less than required (Table 3).
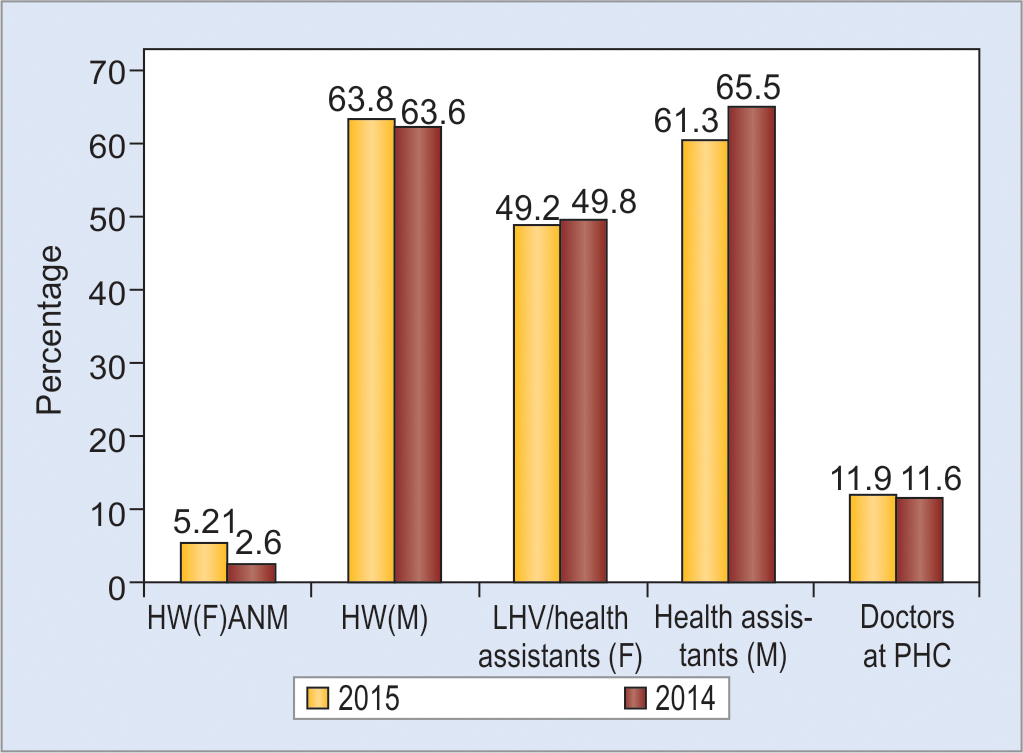
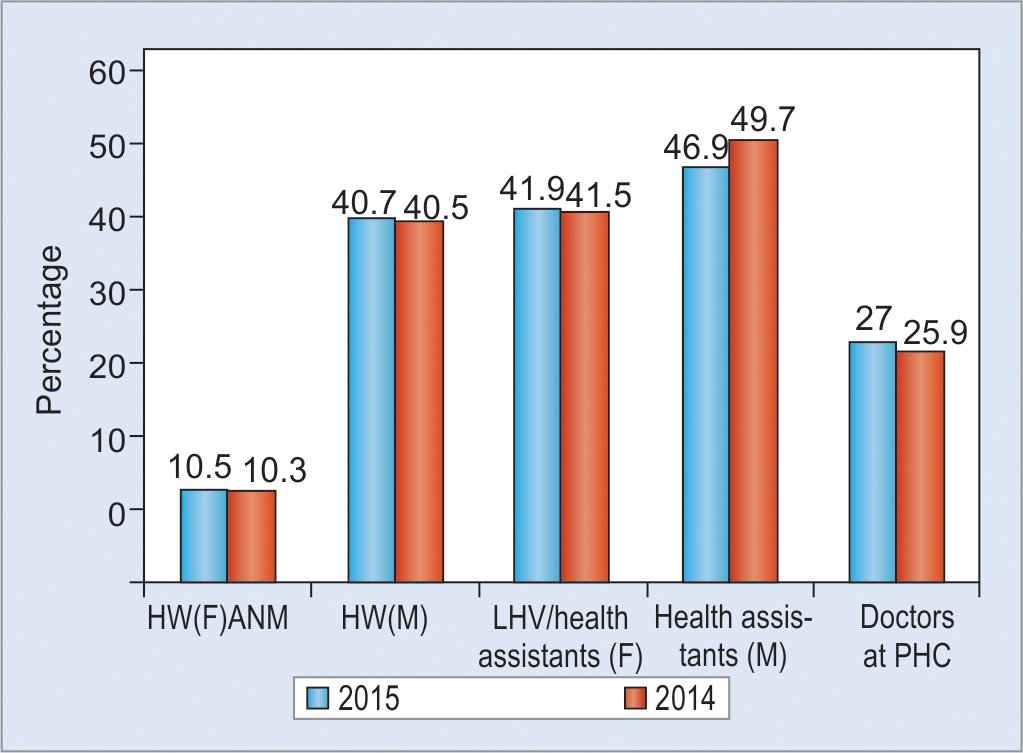
This production is not equal across the states, leading to unequal distribution of doctors. Medical colleges are unevenly spread across the states and also present wide disparities in the quality of education. Only 193 of the 640 districts have a medical college, while the remaining 447 districts do not have any medical teaching facilities. As on March 31, 2015, there were 153,655 subcenters, 25,308 primary health centers (PHCs), and 5,396 community health centers (CHCs) functioning in the country. While the subcenters, PHCs, and CHCs have increased in number in 2014–2015, the current numbers are not sufficient to meet their population norm. Of 25,308 PHCs, 799 have 4+ doctors, 770 have 3 doctors, 2,041 are without any doctors, 9,649 are without lab technicians, and 5,553 are without pharmacists; 6,436 PHCs have lady doctors. A total of 10,237 PHCs have AYUSH facility. Bihar has the maximum number of AYUSH facilities of 1,384. The number of ANMs at subcenters and PHCs has increased from 133,194 in 2005 to 212,185 in 2015, which amounts to an increase of about 59.3%. As on March 31, 2015, the overall shortfall in the posts of health worker (female)/ANM at subcenters and PHCs was 5.21% of the total requirement. Because of the above-mentioned facts, there are only 19 health workers (6 doctors and 13 nurses and midwives) per 10,000 people in India, against a World Health Organization recommended norm of 25 health workers (doctors, nurses, and midwives). Such a skewed distribution results in large gaps in demand and availability, particularly for government health care facilities, which are represented in Tables 4 and 5 and Graphs 2 and 3.
Table 2: Current status of health manpower in various countries
Source: World Health Organization (WHO). World Health Statistics 2015. Geneva: WHO; 20113
Table 3: Number of institutions and admission capacity of paramedical staff
| Courses | No. of institutions | Admission capacity |
| General nurse midwives | 2,865 | 115,844 |
| ANMs | 1,853 | 52,479 |
| Pharmacists | 723 | 43,300 |
Source: CBHI: Ministry of Health and Family Welfare (MOHFW). Rural Health Statistics Report 2014–2015. New Delhi: MOHFW, Government of India; 20115
Table 4: Shortfall against requirement for existing centers
Various reasons for shortfall in health manpower are skewed production of health manpower, uneven human resource deployment and distribution, disconnected education and training, lack of job satisfaction, professional isolation, and lack of rural experience. The 12th Plan should aim to expand facilities for medical, nursing, and paramedical education; create new skilled health worker categories; enable AYUSH graduates to provide essential health care by upgrading their skills in modern medicine through bridge courses; establish a management system for human resource in health to actualize improved methods for recruitment, retention, and performance; put in place incentive-based structures; create career tracks for professional advancement based on competence; and, finally, build an independent and professional regulatory environment.8
SKILLED HEALTH WORKERS
Our health system needs three basic categories of human resource in sufficient numbers and quality. Under each of these four categories, there is scope for expanding the existing nature and functions of designated professionals for that category and also for increasing the depth of training/retraining to make it relevant to national health goals. The three categories and the required nature of expansion in their scope are listed below.
Table 5: Status of medical and paramedical staff in 2005 and 2015
Source: Ministry of Health and Family Welfare (MOHFW). Rural Health Statistics Report 2014–2015. New Delhi: MOHFW, Government of India; 20115
Graph 2
Shortfall against requirement for existing centers. Source: Ministry of Health and Family Welfare (MOHFW). Rural Health Statistics Report 2014–2015. New Delhi: MOHFW, Government of India; 2011.5 HW, health worker; LHV, lady health worker
Graph 3
The shortage figure for doctors relates to doctors at PHCs. Source: Ministry of Health and Family Welfare (MOHFW). Rural Health Statistics Report 2014–2015. New Delhi: MOHFW, Government of India; 2011.5 HW, health worker; LHV, lady health worker
Medical Graduates
Undergraduate teaching should aim to produce clinicians who can independently manage the case load in a primary care facility. Ayurveda, Yoga and naturopathy, Unani, Siddha, and Homeopathy doctors can be trained through short bridge courses to manage essential health care in primary care settings. Doctors deployed in primary and secondary health facilities need to be multiskilled, so that they can manage day-to-day conditions relating to obstetrics, anesthesia, psychiatry, pediatrics including neonatology, and trauma care.
Medical and Surgical Specialists
The discipline of family medicine should be introduced in all medical colleges so that qualified specialists in this discipline can effectively manage most of the medical problems encountered at the primary level, and referral to specialists occurs only when necessary. Such recommendations have been made earlier too by the Mehta Committee in 1983.9
Paramedical Workers for Health Facilities
Studies suggest that in primary care, appropriately trained nurses can produce as high a quality of care and achieve as good a health outcome for patients as doctors Paramedical and allied health care professionals constitute the base of the pyramid and are required in adequate numbers for optimal performance of teams. The issues in question are shortages, absence of many required cadres, and underutilization of their potential. For example, in the context of hospitals, a survey by the Federation of Indian Chambers of Commerce and Industry in June 2011 identified five skillsets that need immediate attention, namely, dialysis technicians, operation theater/anesthesia technicians, paramedics, lab technicians, and patient care coordinator cum medical transcriptionists. The existing paramedical human resource need to be suitably trained, clinically empowered, and deployed to enable optimal utilization of their services.10
EXPANSION OF MEDICAL, PUBLIC HEALTH, NURSING, AND PARAMEDICAL EDUCATION
The strengthening of existing institutions, and also the creation of new ones, in terms of infrastructure and faculty is required for training of new health workers and reskilling of existing human resources. For this, a feasible and cost-effective option is to upgrade existing district hospitals and CHCs into knowledge centers, where medical and paramedical teaching and refresher courses can occur side-by-side with patient care.
Setting up 30 new medical colleges with public financing, preferentially in states with larger gaps. This step alone would increase undergraduate medical seats from 41,569 to 63,000 and postgraduate seats from 20,868 to 31,000.
Strengthen state government medical colleges and central government health institutions with the triple objective of increasing the intake of undergraduate and postgraduate candidates by 20,000 and 10,000 respectively; providing superspecialty and other specialized services for patient care at these tertiary care centers; and setting up degree programs for nursing and paramedical courses within these institutions, in case none exists.
Setting up paramedical education courses in 149 government medical colleges, in addition to initiating paramedical institutions in 26 states. Strengthening and upgradation of government pharmacy institutions.
MANAGEMENT SYSTEM FOR HUMAN RESOURCE IN INDIA
The shortage of health personnel against the requirement across the country as per the Bulletin of Rural Health Statistics, 2010 is 63% for specialists, 19% for doctors, and 7% for ANMs. Reasons for the same are attributed to delays in recruitment and to postings not based on workload or sanctions. Though most of the public health workers and medical officers are recruited, deployed, and managed by the states, the central government can suggest model human resource policies and minimum standards of workforce management for better retention and performance. These guidelines should include the following strategies:
The Indian Public Health Standards should be taken as the guiding principle for sanctioning posts, though the actual posting may depend on caseloads.
Recruitment should be decentralized with a quicker turnaround time and preference must be given to residents of the region of proposed deployment.
Fair and transparent system of postings and timely promotions.
Financial and nonfinancial incentives (like preferential eligibility for postgraduate courses, promotions, subsequent choice of postings) for performance and service in remote areas.
Measures to reduce professional isolation by preferential access to continuing medical education and skill upgradation programs, as well as back-up support on telemedicine (Internet or mobile based) and by networking of professionals working in similar circumstances (Flow Chart 1).11

