CASE REPORT | https://doi.org/10.5005/jp-journals-10055-0090 |
Proliferating Trichilemmal Cyst Presenting as a Limbal Mass
1,2,4Department of Ophthalmology, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, Punjab, India
3Department of Pathology, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, Punjab, India
Corresponding Author: Pawan Prasher, Department of Ophthalmology, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, Punjab, India, Phone: +91 9646104858, e-mail: pawanprasher@yahoo.com
How to cite this article Nagpal N, Kaur I, Manjari M, et al. Proliferating Trichilemmal Cyst Presenting as a Limbal Mass. AMEI’s Curr Trends Diagn Treat 2020;4(1):41–43.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Limbal mass may present as a diagnostic dilemma to the ophthalmologist. Histopathology of the excised mass plays a critical role in establishing the diagnosis and has prognostic implications. Herein, we report a rare case of trichilemmal cyst presenting as a limbal mass involving the bulbar conjunctiva. A 25-year-old female presented with symptoms of ocular discomfort associated with a whitish-opalescent, mildly elevated, nodular nasal limbal lesion measuring 5 × 4 × 3 mm in greatest dimensions in left eye. Excisional biopsy of the mass, along with excision of surrounding 2 mm healthy conjunctiva followed by mitomycin 0.04% application, was carried out. Histopathology features were characteristic of trichilemmal keratinization, a heretofore undescribed metaplasia of the conjunctival epithelium. No recurrence was seen up to 3 years of follow-up.
Keywords: Conjunctiva, Limbal nodule, Trichilemmal cyst.
INTRODUCTION
Trichilemmal cyst, also known as pilar cyst, is a common cyst that arises from a hair follicle.1 The cysts are lined by smooth flattened epithelium and filled with keratin, a protein component found in hair, nails, and skin. These are usually benign in nature; however, malignant transformation with high recurrence rates, local invasion, and metastases have been rarely described.2
Usually, they are located in the scalp, eyelid margin, or caruncle, where hair follicles are present. Both trichilemmal and epidermal cysts are keratinous cysts and usually have similar clinical presentation. Approximately 20% of epithelial cysts are trichilemmal cysts, and 80% are epidermal. However, these cysts differ significantly in their manner of keratinization on histopathology.1 Herein, we report a rare case of trichilemmal cyst presenting as a limbal mass involving the bulbar conjunctiva which is an unusual location for this cyst to occur. To the best of our knowledge, only one case of trichilemmal cyst of conjunctiva has been previously reported in the literature.3
CASE DESCRIPTION
A 25-year-old female presented with gradually increasing mass in the left eye for over one month. It was associated with redness, mild irritation and watering. There was no history of trauma or any similar episode in the past.
Before presenting to us, she had received treatment elsewhere in the form of topical antibiotics, lubricants, and steroids; however, there was no improvement in the mass or associated symptoms. Visual acuity on presentation was 20/20 in both eyes. Slit lamp examination showed an elevated nodular mass measuring 5 × 4 × 3 mm at the nasal limbus of the left eye. The mass had gelatinous, pearly white appearance in the center with dilated vessels in the peripheral part. There was associated epithelial irregularity of the adjacent cornea (Fig. 1). The mass appeared to be mobile over the underlying tissues. The rest of ocular and systemic examination was unremarkable. Under local peribulbar anesthesia, an excisional biopsy of the mass along with 2 mm of surrounding healthy conjunctival tissue was performed, and the specimen was sent for histopathological examination. The excision was followed by application of 0.04% mitomycin-C application for 2 minutes over the scleral bed. Postoperatively, the patient was put on topical moxifloxacin eye drops four times daily, prednisolone eye drops four times daily, and ciprofloxacin eye ointment at bedtime. There was an evidence of early pyogenic granuloma formation at 2 weeks follow-up visit, which resolved on increasing the frequency of topical prednisolone eye drops to every 2 hours. Histopathological examination of the submitted specimen showed islands of squamous cells with keratin filled cysts in the substantia propria. Cysts were lined by stratified squamous epithelium (Fig. 2). These squamous cells showed abrupt keratinization, without any granular layer, consistent with trichilemmal keratinization with no evidence of atypia (Fig. 3A). At 3 months postoperative visit, the patient was asymptomatic, and slit lamp examination showed well healed conjunctiva at the site of excision with resolution of symptoms of ocular discomfort (Fig. 3B). The patient has been followed up for over 5 years now with no evidence of recurrence of the mass.
DISCUSSION
Limbus is the region of the eye between the cornea on one side and the sclera on the other which houses stem cells. A limbal nodule often presents as a difficult clinical, histopathologic, and therapeutic challenge.4 These lesions are transitions between inflammation, inflammatory hypertrophies, and true neoplasms thus posing a diagnostic challenge.5 As patient presented with features of watering and foreign body sensation, this could be confused with conditions like nodular episcleritis, scleritis or inflamed pterygium which was ruled out on clinical examination due to its unusual physical appearance. Neoplastic growth in limbus are the most common among growths of cornea and conjunctiva owing to the transition nature of the limbus. Squamous cell carcinoma is the most common carcinoma of limbus that can easily be confused with reactive hyperproliferative lesions like trichilemmal cyst. Histopathology plays a critical role in such scenarios not just to establish the diagnosis but also to explain the future prognosis to the patient.
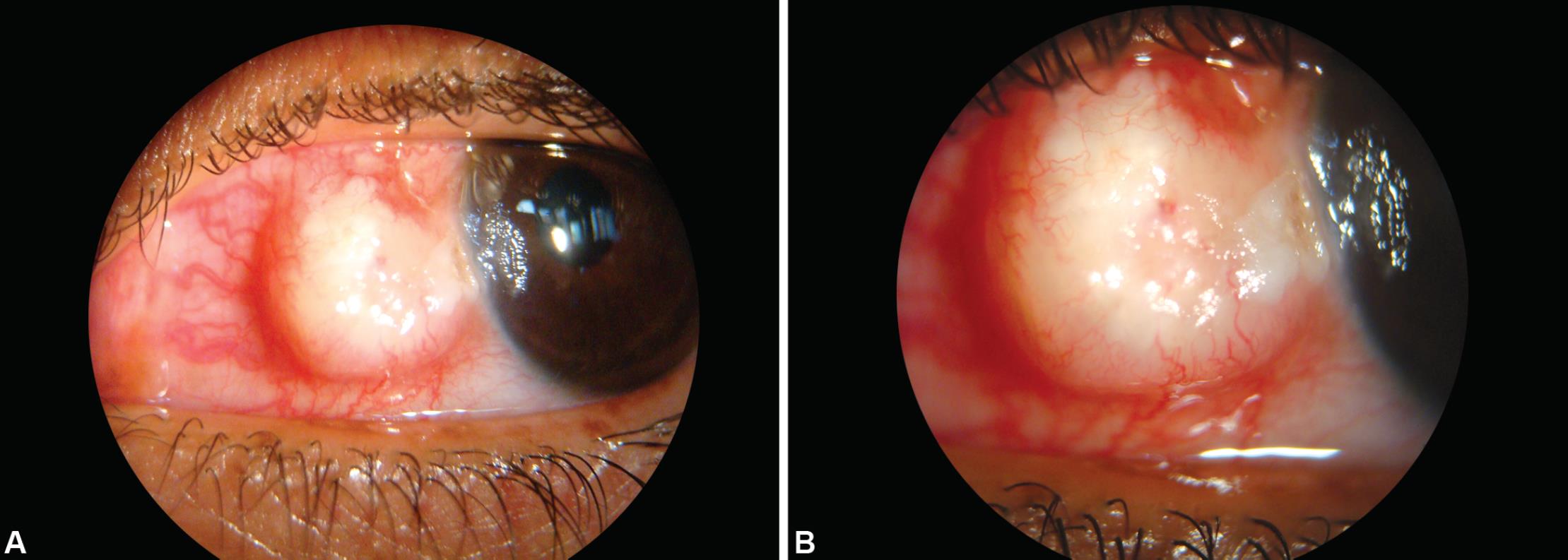
Figs 1A and B: (A) Slit lamp photograph at presentation showing an elevated nodular mass at nasal limbus of left eye; (B) A gelatinous central mass with surrounding radiating vessels in the periphery can be appreciated at higher magnification

Figs 2A and B: Histopathological examination showing: (A) Cysts were lined by stratified squamous epithelium with abrupt keratinization, without any granular layer, consistent with trichilemmal keratinization and no evidence of atypia; (B) In other areas, islands of squamous cells with keratin-filled cysts are seen in the substantia propria
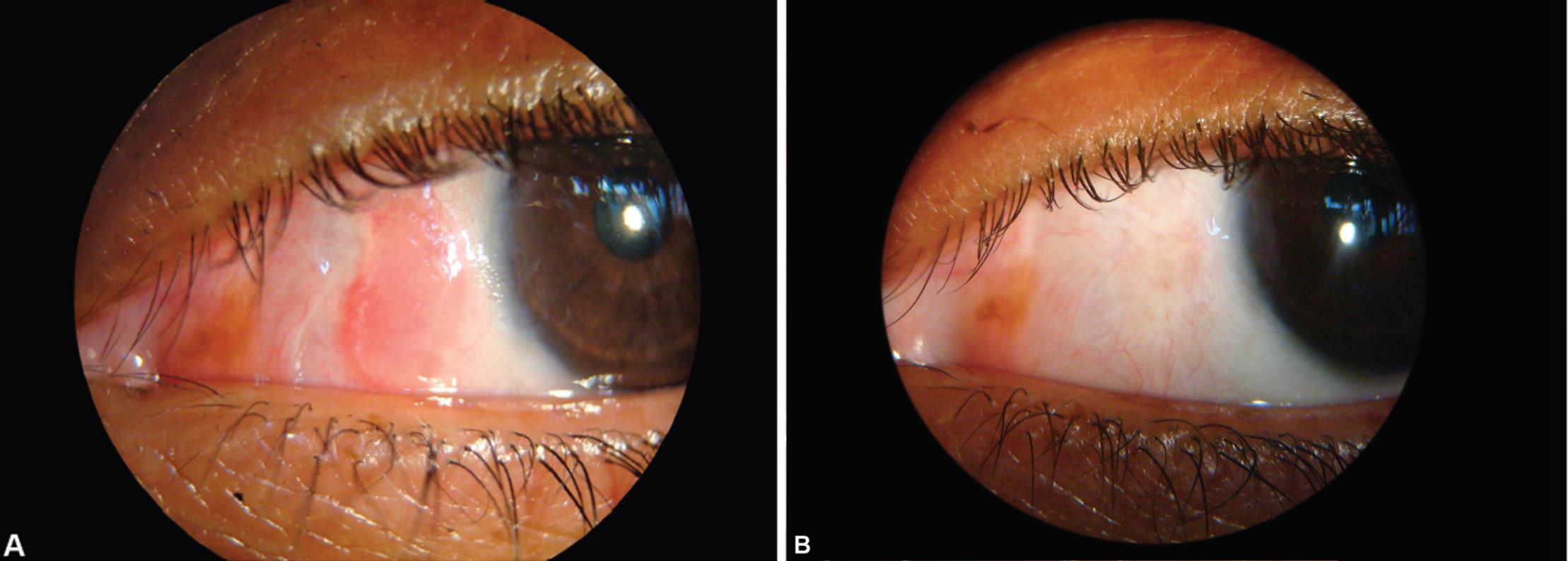
Figs 3A and B: (A) Slit lamp picture showing early pyogenic granuloma formation on postoperative day 7; (B) A well-healed conjunctiva at the site of excised mass on 3 months postoperative visit
A trichilemmal cyst, also known as wen, pilar cyst or isthmus-catagen cyst arises from a hair follicle. Although most often found on the scalp, they can also occur on other parts of the body such as the upper lip, palpebral conjunctiva, caruncle, and pulp of the index finger.6,7 The mechanism of formation of proliferating trichilemmal cyst in the current case is not clear; however, we speculate it could be a result of implantation of epithelium of eyelid skin while rubbing or by migration from the caruncle.
These cysts are similar to epidermal cysts, both being keratinous cysts usually having a similar presentation. However, histologically, the cells undergo abrupt transition from stratum spinosum to keratinized layer without the formation of granular layer, thus differing from epidermal cysts.8,9 Rarely, trichilemmal cysts have undergone malignant transformation.10 In our case, the cyst showed basal cell hyperplasia without cell atypia or mitosis, which helped out in ruling out the diagnosis of squamous cell carcinoma. To the best of our knowledge, only one more case of nasal conjunctival trichilemmal cyst has been reported in the literature, which extended from the caruncle and was an older aged female. Also this case was from a different geographical coastal area in South India, when compared to the hot and dry climate of Punjab for the current patient, with a longer history of 3 years.3 To the best of our knowledge, no similar case in a younger age-group has been reported as a separate limbal mass.
CONCLUSION
This case report highlights the need for considering proliferating trichilemmal cyst as a differential diagnosis of the limbal nodule. Radical surgical treatment and precise histological analysis are essential for the appropriate management of these challenging cases. A close cooperation between the treating ophthalmologist and the pathologist cannot be overemphasized for accurate diagnosis, treatment, and follow-up planning.
REFERENCES
1. Meena M, Mittal R, Saha D. Trichilemmal cyst of the eyelid: masquerading as recurrent chalazion. Case Rep Ophthalmol Med 2012;2012: 261414. DOI: 10.1155/2012/261414.
2. Garetto F, Morozzo G, Morozzo U, et al. Recurrent proliferating trichilemmal cyst of the scalp. G Ital Dermatol Venereol 2018;153(1):107–110.
3. Lai TF, Huilgol SC, James CL, et al. Trichilemmal carcinoma of the upper eyelid. Acta Ophthalmol Scand 2003;81(5):536–538. DOI: 10.1034/j.1600-0420.2003.00132.x.
4. Farah S, Tad D, Baum, et al. Tumors of cornea and conjunctiva. In: ed. J, Albert G, Azar ed. Principles and Practice of Ophthalmology.vol. 2, Philadelphia: W.B. Saunders Co; 2000. pp. 1002–1016.
5. Duke-Elders S. Diseases of the outer eye Vol. VIII. part 2. cornea and sclera henry Kimpton. System of Ophthalmology. St Louis: CV Mosby; 1965. pp. 1144–1241.
6. Jakobiec FA, Mehta M, Sutula F. Keratinous cyst of the palpebral conjunctiva. Ophthal Plast Reconstr Surg 2009;25(4):337–339. DOI: 10.1097/IOP.0b013e3181aada9a.
7. Jakobiec FA, Mehta M, Greenstein SH, et al. The white caruncle: sign of a keratinous cyst arising from a sebaceous gland duct. Cornea 2010;29(4):453–455. DOI: 10.1097/ICO.0b013e3181b55b5c.
8. Elder D, Elenitsas R, Ragsdale B. Tumors of the epidermal appendages. In: ed. D, Elder R, Elenitsas C, Jaworsky ed. Lever’s Histopathology of the Skin. Philadelphia, Pa, USA: Lippincott Williams and Wilkins; 1997. pp. 749–779.
9. Satyaprakash AK, Sheehan DJ, Sangüeza OP. Proliferating trichilemmal tumors: a review of the literature. Dermatol Surg 2007;33(9):1102–1108. DOI: 10.1097/00042728-200709000-00011.
10. Kadri R, Parameshwar D, Ilanthodi S, et al. Trichilemmal cyst of the bulbar conjunctiva: a rare presentation. Middle East Afr J Ophthalmol 2013;20(4):366–368. DOI: 10.4103/0974-9233.119999.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.